Introduction
Spleen is one of the most commonly injured organs after abdominal blunt injury. Nonsurgical management (e.g., transarterial embolization of splenic artery [SA]) is feasible and safe in patients with hemodynamical stability with a spleen injury. SA usually arises from the celiac axis, whereas its varying origins (e.g., common hepatic or superior mesenteric artery) are occasionally reported [1]. A very uncommon case of SA originating from proper hepatic artery (PHA) is reported here, and the spleen injury was treated with transarterial embolization.
Case presentation
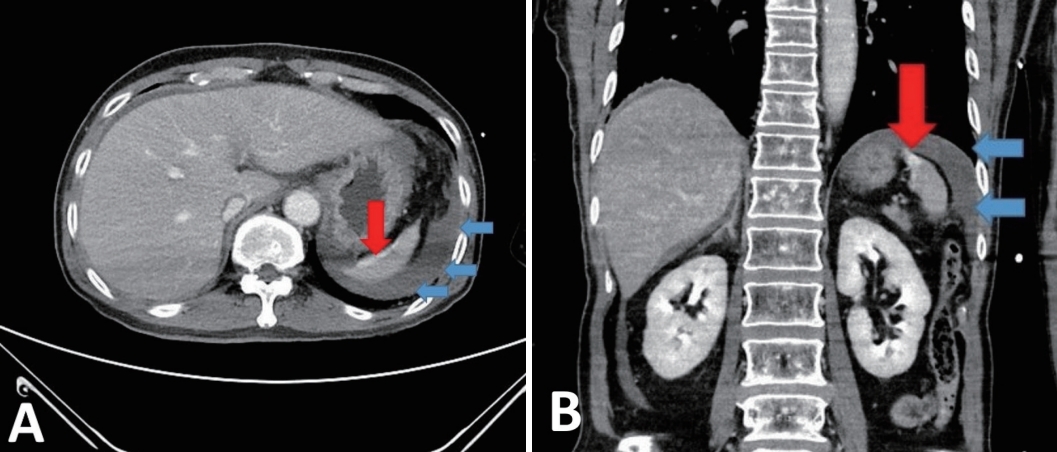
A 57-year-old male patient, who was a driver in a rollover car accident, was referred with chest wall pain. The patient presented tenderness on the bilateral chest wall, whereas the patient’s abdomen was soft and nontender. The patient was hemodynamically stable with a blood pressure of 101/60 mmHg, a pulse rate of 125 beats per min, and a hemoglobin level of 9.9 g/dL. The patient’s injury severity score was 17. The computed tomography revealed the Grade 2 spleen laceration with contrast blush (Fig. 1).
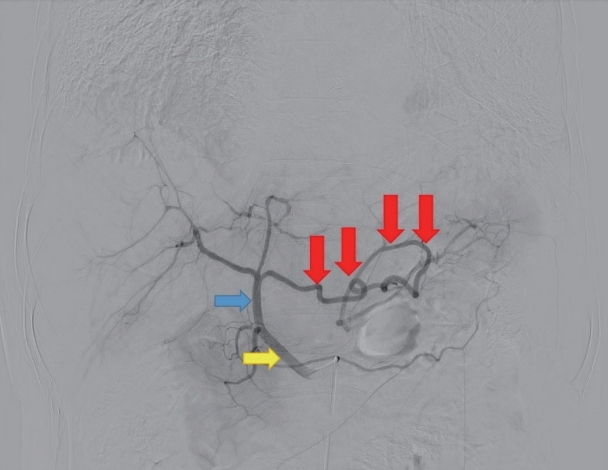
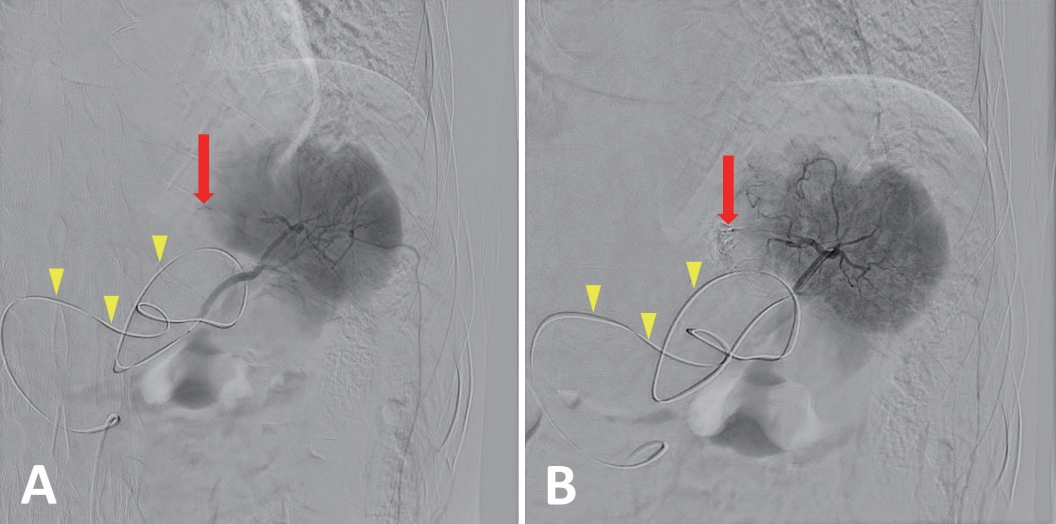
The patient was hemodynamically stable, and diagnostic angiography with therapeutic SA embolization were shortly performed afterward. In angiography, the guidewire entry to the celiac trunk was demanding and a variant SA arising from PHA was noted. Hence, SA cannulation was achieved via PHA (Fig. 2). The culprit SA branch was embolized using n-butyl cyanoacrylate (Fig. 3). The 1.9F, 130-cm-long catheter and a 0.016-in, 165-cm-long microguidewire were used during the procedure. The total duration of transarterial embolization was 67 min. The patient started the diet on hospital day 3 and was discharged on hospital day 12 without any complications.
Discussion
Nonoperative management is the treatment standard of traumatic splenic injury in patients with hemodynamical stability. SA embolization has become the treatment of choice especially for those with contrast extravasation in splenic injury sites [2-4]. However, the transarterial embolization in patients with splenic injury may become more challenging if the patient has variant SA origin. Several case reports exist for the successful transarterial embolization of patients with variant SA aneurysm whereas the study for patients with a traumatic splenic injury who have variant SA is insufficient.
The SA which originated from PHA is extremely uncommon and has not been reported. Splenic origin concluding that celiac axis, abdominal aorta, and common hepatic or superior mesenteric arteries accounted for 96.6%, 8.1%, and 1.3%, respectively, in a study of 320 cadavers. The knowledge of these variations is important to avoid complications during both surgical and nonsurgical procedures [1,5].
Splenic infarction and abscess are the main SA complications from embolization [4]. However, patients with SA embolization uncommonly suffer from splenic infarction because other vessels (e.g., short gastric arteries or the gastroepiploic arteries) keep feeding the spleen. Most of these patients are asymptomatic and can be managed nonsurgically, even if the splenic infarction or abscess develops. Thus, transarterial embolization deserves to be performed in patients who have variant SA origin even though the procedure may be technically difficult.
In conclusion, transarterial SA embolization may be feasible in patients who have variant SA origin, even though the procedure is more challenging and a longer catheter may be needed compared to those with the usual case. Future studies are needed for transarterial embolization of variant SA in traumatic splenic injury.