Introduction
Various techniques have been developed for percutaneous dilatational tracheostomy (PDT), since its first introduction by Ciaglia et al. in 1985 [
1], followed by the Ciaglia, Grigg, Fantoni, and Percu-Twist methods [
2-
4]. PDT provides advantages over a surgical tracheostomy, including requiring fewer professionals, being faster, and requiring less equipments. As a reason, it has been considered a well-known method at the bedside [
5]. In addition, endotracheal guidance, such as the flexible bronchoscope, has become less necessary with the advancement of PDT [
6]. Therefore, this study aimed to describe the unassisted PDT using Ciaglia Blue Rhino percutaneous tracheostomy set with a
video clip.
Technical methods
Patient position and preparation
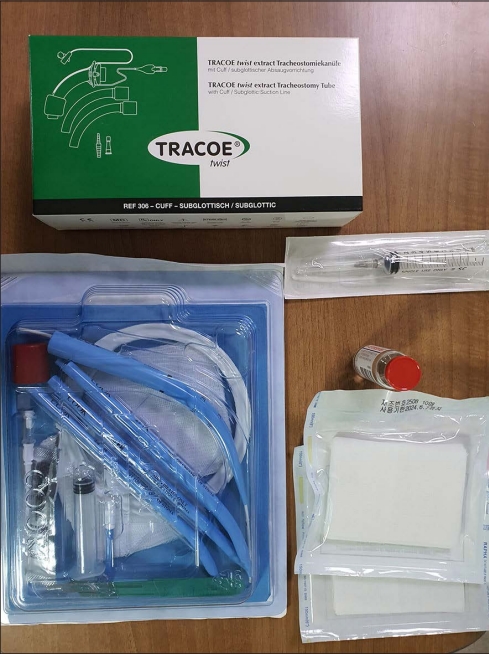
The patient should be placed in the supine position with the pillow beneath the scapulae. It is helpful to expose the anterior neck, but not essential in a specific condition for cervical immobilization. The ventilator setting should be adjusted as needed. Sedatives and a short-acting paralytic agent could be considered necessary to control the adverse movement of the patient. The percutaneous tracheostomy kit (Cook Medical Incorporated, Bloomington, IN, USA), tracheostomy tube appropriate for the patient, and local anesthesia should be prepared at preprocedure (
Fig. 1). To ensure an uninterrupted process and to maintain the airway, the endotracheal tube is adjusted at the T1 level on a chest X-ray (CXR) (
Fig. 2). Thereafter, the anterior neck should be draped after sterilizing it.
Identification of anatomical landmarks
To identify the appropriate tracheostomy site, the anatomical landmarks of the neck should be palpated, including the thyroid cartilage, cricoid cartilage, and sternal notch (
Fig. 3). The optimal site for the tracheostomy tube is between the second and third tracheal rings, i.e., halfway between the inferior border of the cricoid cartilage and sternal notch. The pre-evaluation of the trachea using ultrasound may be useful to determine the precise site of tracheostomy and avoid potential complications in some high-risk patients, such as those with unclear pre-evaluation of anatomical variation, unrecognized vascular variations, and impalpable trachea, such as in patients with obesity or a short neck (
Fig. 4).
Preparation of a PDT product
The Ciaglia Blue Rhino percutaneous tracheostomy introducer set is released. Next, the instruments are sorted as per the PDT process (
Fig. 5). The tracheostomy tube loading dilator and percutaneous tracheostomy dilator are lubricated. After testing the balloon of the tracheostomy tube (TT, T-cannula), a proper loading dilator (21 Fr. Loading dilator) is premounted to the TT (Tracoe medical GmBH, Frankfurt, Germany, 7mm). Connect a syringe filled with some saline to the 15 gauge introducer needle (puncture needle).
Procedure
Procedure steps are as follows:
1. Induce local anesthesia with 2% lidocaine at the puncture site.
2. Perform tracheal puncture, perpendicular to the trachea while aspirating the needle with the bevel facing down. Simultaneously hold the trachea for immobilization with the other hand.
3. Verify the air leakage and bubbles and halt the needle insertion.
4. Gently insert the guidewire with the J tip facing downward.
5. Remove the introducer needle alone, keep the wire in situ.
6. Insert an introducer dilator (stiff dilator) along the wire.
7. After making an incision at the insertion site, a tract around the guide wire is smoothly dilated.
8. Insert the dilator assembly (the percutaneous tracheostomy dilator with a guiding catheter) along the wire. To dilate and insert the skin level mark of the dilator. If necessary, gently move the dilator back and forth a few times.
9. Remove the dilator assembly.
10. Insert the premounting T-cannula along to the wire.
11. When the T-tube is properly mounted, the obturator and wire are removed.
12. Inflate the balloon to secure the T-cannula.
13. Connect the ventilator circuit directly to the T-cannula. Confirm appropriate ventilation through a secured tracheostomy cannula (Fig. 6).
14. A dedicated band is cut to fit the patient’s neck and fixed to the T-cannula.
15. The oral endotracheal tube is removed.
16. Confirm the CXR after PDT (Fig. 7).
Discussion
The PDT can be dangerous when the tube and needle are inserted blindly, especially in perioperative tracheal bleeding, regardless of the bleeding quantity. Therefore, the unassisted PDT should be performed by an experienced and well-trained physician. If necessary, the pre-evaluation using ultrasound for neck anatomy may be helpful. The needle should be initially introduced into the appropriate site, and the guidewire must hold up in the trachea while performing an unassisted PDT. These two factors are considered crucial for the uneventful execution of unassisted PDT.