Internal jugular central venous catheterization: a focus on the procedure
Article information
Abstract
Central venous catheterization (CVC) is very common procedure in the emergency department and intensive care unit. Although patients undergoing CVC may have various indications and contraindications for this catheterization, the procedure is typically similar, regardless of the route. However, site-specific precautions also exist. This report describes the overall procedure for CVC with access by the internal jugular vein. Neurologic complications such as stroke and cranial air embolism, as well as mechanical complications such as hemopneumothorax and hematoma, can occur related to the internal jugular venous approach to CVC. Clinicians should be aware of these concerns for these patients population.
Introduction
Central venous catheterization (CVC) through the internal jugular (IJ) vein is very common procedure in the emergency department and intensive care unit. The clinicians should be aware of the accurate and various indications, contraindications, and precautions for patients undergoing CVC. Most indications and contraindications (primarily relative contraindications) are common to CVC, regardless of the route of access, but some specific complications or precautions exist related to the access route. This article focuses on the CVC via the IJ vein. For general information of CVC, ultrasound (US) use and underlying principles, the reader is referred to other studies, as these points are not addressed herein.
General principles and anatomy
The IJ vein combines with the subclavian vein that leads to the innominate (brachiocephalic) vein and serves as a vessel that flows the circulated blood from head and neck. Although generally no valves are present in the central veins, a valve is present in the IJ vein, which can act as an obstacle during catheterization and may be damaged during the procedure [1]. The IJ vein lies superficial and lateral to the carotid artery in the carotid sheath in the supine position. In some cases, however, rotation or overlapping of the vessels may exist, which is why US-guided catheterization is necessary in the IJ vein area. [2,3].
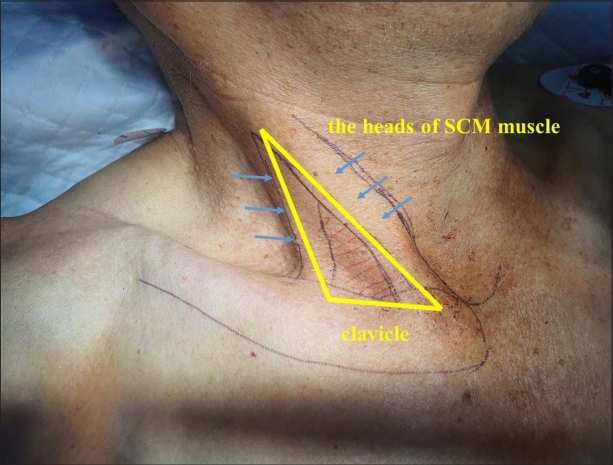
In general, the diameter of the right IJ vein is larger than that of the left. The diameter can be increased during end expiration, in the Trendelenburg position, during the Valsalva maneuver, or while humming, which can be used to increase the success rate of CVC (4-6). An anatomic triangle composed of the two heads of the sternocleidomastoid (SCM) and the clavicle is a key location to understand the vascularity (Fig. 1). Typically, the IJ vein lies at the triangle apex. The optimal length from the insertion site to the proper depth of the catheter tip (superior vena cava–right atrial junction) estimated by transesophageal echocardiography is approximately 18 cm [7].
Advantages, disadvantages, site-specific indications, and contraindications
When approaching the IJ vein, it is relatively easy to identify external landmarks, with a high success rate using US guidance. The rate of catheter malpositioning is relatively low [8,9]. The incidence of iatrogenic pneumothorax is low, and hematoma formation is easy to be discovered and controlled. Bleeding due to arterial puncture can be controlled with ease because compression is possible. Although there is no indication that only the IJ vein should be selected, it is generally a suitable route for transvenous pacemaker insertion or central venous pressure monitoring. If an indwelling central catheter is already present in the IJ vein, the lactate concentration obtained from here reflects overall perfusion and can replace the arterial blood lactate (strong correlation, r=0.84; average difference in values: –0.8±5.9) [10].
Disadvantages are a higher risk of infection and thrombus formation than for the subclavian vein (SV). The IJ CVC-specific contraindications are as follows: traumatic swelling at the cervical region, anatomic distortion of intended IJ venous puncture site due to surgery, history of radiation therapy to the neck, and preexisting carotid artery disease, such as atherosclerotic plaque (relative contraindication) (Fig. 2).
Routes of approach
The three approaches to IJ CVC are central, anterior, and posterior. This article describes the central approach in detail. In the anterior approach, the needle is inserted anterior to the sternal head of the SCM, aimed to the ipsilateral nipple. In the posterior approach, the puncture is initiated at the posterior edge of SCM between its origin and insertion at the clavicle and advanced toward the suprasternal notch. Caution is needed not to puncture the external jugular vein. This approach starts relatively high in the neck, with less risk of hemothorax or pneumothorax [11].
Technical methods
The right side is preferred for IJ CVC because the diameter of right IJ vein is typically larger than that of left and the right side has a straight anatomic path to the superior vena cava (12). Patient position is critical for the procedure, with the head rotated to 15°–30° opposed to the CVC side. Head rotation >40° is not recommended because of the potential for the vessels to overlap.
With the patient in a monitoring room, US is used to verify the vessel structures and variations to confirm whether it is an appropriate location for CVC. Recently commercial CVC kits are used widely. Place the accessories of the kit in a sterile set after the full sterile barrier precaution. At this time, care must be taken not to spill the accessories. In general, the safety syringe and long puncture needle for venipuncture, a dilator, one- or multi-lumen catheter, a guidewire, a catheter rubber clamp are included in the kit. The suture silk, aseptic dressing materials, local anesthetics with lidocaine or bupivacaine, the syringe for the anesthetic, scalpel are maybe also required. Each lumen of catheter should be flushed with sterile normal saline. After flushing, clamp the lumen except for one port (usually the largest port) from which the guidewire will come out to minimize the air entry or bleeding through the catheter. The puncture needle and the introducer syringe should be flushed before the insertion. It is recommended that the bevel of the needle and the scale of the syringe should be aligned. This is why it is easy to recognize when the direction is slightly rotated immediately after insertion (Video 1).
After full-body, sterile draping and catheter preparation, the optimal puncture site is decided under US guidance, typically the triangle apex. On US, the IJ vein lies superficial and lateral—but not always—to the carotid artery, is oval in shape, has a thin wall, and is compressed with gentle pressure (Fig. 3). If it is not compressed, the structure may be misidentified or a thrombus may exist, which may not be suitable for cannulation. After site confirmation, next steps are to inject the local anesthetic with lidocaine or bupivacaine and, because lidocaine can cause dysrhythmias, to aspirate the syringe to determine if the needle punctured arteries or veins pre-administration.

(A) Right internal jugular (IJ)vein and carotid artery (CA). Note that internal jugular vein has thin wall and oval shape. (B) The internal jugular vein can be compressed by the gentle compression.
In central approach, the needle puncture is initiated at slightly lateral to the carotid pulse (Fig. 4). The needle is inserted at the triangle apex while maintaining an entry angle of 30° and aiming the needle tip toward the ipsilateral nipple. The syringe needle is inserted slowly while maintaining negative pressure. When blood flashback appears, advancing is stopped and the syringe is removed to verify the vessel is pulsatile. If arterial puncture is suspected (bright red, pulsatile), it should be removed immediately and compressed. If drawn blood is dark and non-pulsatile, it is highly likely to be venous blood. However, if a patient is in shock from severe bleeding or severe desaturation, blood may appear dark or non-pulsatile, so caution is needed.

The central approach to internal jugular venous catheterization. The needle should be aimed toward the ipsilateral nipple. The carotid pulsation can be felt at the blue star point.
Once vein puncture is confirmed, a guidewire is introduced. During this procedure, the needle must be well stabilized not to move freely. After an appropriate depth of guidewire insertion, the needle is removed. Insertion too deep may cause myocardial irritability and subsequent dysrhythmias and, rarely, cardiac perforation can occur, leading to cardiac tamponade (Fig. 5). Therefore, cardiac monitoring is required. If any resistance is felt during the guidewire insertion, the insertion is never forced because the guidewire can be broken (Fig. 6).

(A) Central venous catheterization via the right internal jugular vein. (B) During guidewire insertion, multiple premature ventricular complexes were shown on the electrocardiogram monitor.

A broken guidewire. If any resistance is felt during guidewire insertion or removal, the guidewire and the needle should be removed as a single-unit.
The operator can make a small incision for an easy path for the dilator. The dilator is inserted to a depth sufficient to penetrate the blood vessel through the guidewire and then removed. The catheter is inserted over the guidewire and advanced smoothly without resistance when entering the catheter. If any resistance is felt, it is recommended to check the location with US or retry after removal. Once the catheter is inserted to an appropriate depth, the guidewire is removed and all lumens are flushed with sterile saline. The operator ensures that unused ports are capped and secures the catheter with suturing, and then cleans the insertion area and finishes with a simple dressing. Care should be taken to prevent air from entering through a catheter or needle during catheterization.
After CVC, chest radiography is performed to check the catheter tip location and for complications and malposition (Fig. 7). An appropriate tip position is the superior vena cava–right atrial junction (Fig. 8). The procedures were recorded at the Dankook University Hospital Trauma Center (Video 2); a 7-Fr triple-lumen ARROW CVC (Arrow, Zdar, Czech Republic) was used.
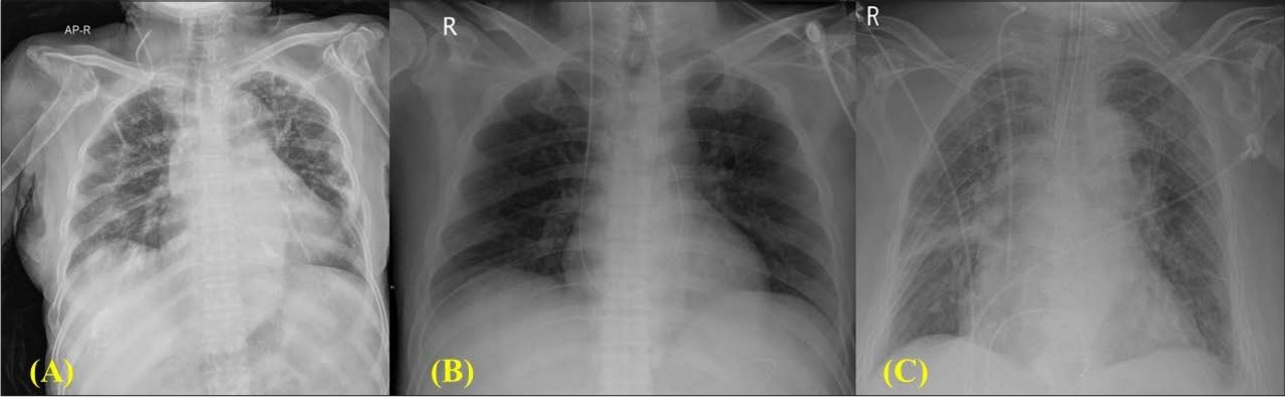
Chest radiographies after central venous catheterization show (A) catheter tip malposition; (B) retained guidewire; and (C) insertion too deep in the heart.
Site-specific complications
Overall 15% of CVC patients experience complications [13]. Most IJ CVC complications are similar to those with SV CVC. Although pneumothorax mainly occurs in the SV approach, it can also occur with the IJ approach, with an incidence of approximately 0.2% [13]. Air embolism is rare but fatal and can occur during the catheter insertion or removal [14]. Transmission of 100 mL/second of air through 14-gauge needle is possible, with a 5-cm H2O pressure difference [15]. If air embolism occurs within the cranium (cerebral air embolism), emergency hyperbaric oxygen therapy is required.
Myocardium perforation and cardiac tamponade are possible [16]. If cardiac tamponade causes shock, emergency pericardiocentesis is needed. Neck hematoma is a common complication site-specific to the IJ CVC but easy to be discovered and controlled. Several neurologic complications are reported, as phrenic nerve damage, iatrogenic Horner syndrome, brachial plexus injury, and inadvertent CVC into the spinal canal thecal space [17-19]. Valve incompetence may occur, of uncertain clinical importance [20]. Inadvertent carotid artery insertion requires referral to a vascular surgeon with the catheter in place because removal causes stroke, leading to morbidity or mortality [21-23]. Finally, rates of central line–associated bloodstream infections has decreased with US-guided IJ CVC [24].
Conclusion
CVC through the IJ vein is a common approach; however, clinicians must be aware of site-specific techniques and concerns.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Supplementary material
Supplementary data including one video can be found with this article online at www.traumaimpro.org.
Video 1.
The preparation of central venous catheterization.
Video 2.
The procedure of central venous catheterization through the right internal jugular vein.