Isolated acute hemorrhagic cholecystitis in liver cirrhosis after blunt trauma
Article information
Abstract
Isolated acute hemorrhagic cholecystitis (AHC) after blunt trauma is extremely rare. Thus, alcoholic liver cirrhosis can be a risk factor for this type of injury. The use of point-of-care ultrasound as a monitoring tool for suspicious gallbladder injuries facilitates rapid recognition and decision-making. Therefore, laparoscopic cholecystectomy was recommended for treating traumatic AHC in patients with hemodynamically stable liver cirrhosis.
Introduction
Gallbladder (GB) injuries from blunt abdominal trauma are rare with a reported incidence of 0.5%±0.6% of all intra-abdominal injuries [1]. The isolated GB injuries are even more unusual. Less than 2% of traumatic GB injuries are without concomitant abdominal pathology [2]. A unique case of isolated acute hemorrhagic cholecystitis (AHC) in a patient with alcoholic liver cirrhosis after blunt trauma has been described here.
Case Presentation
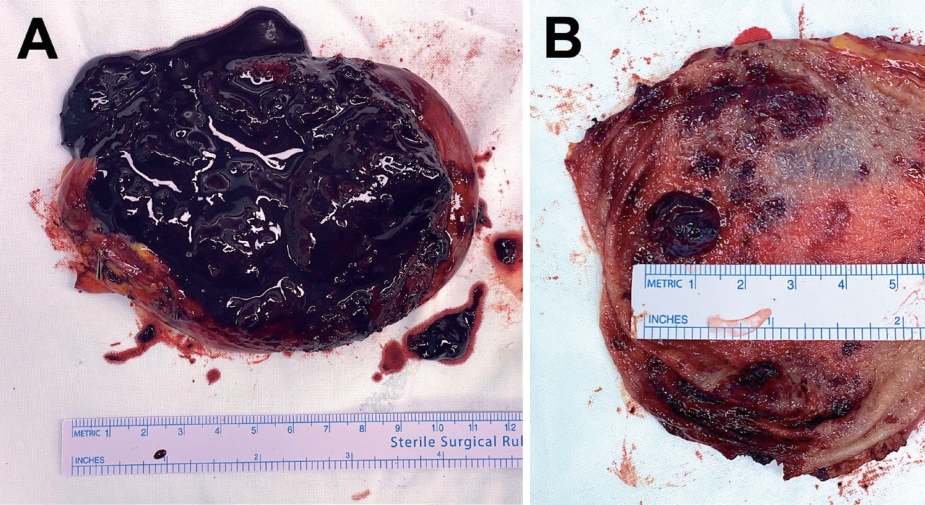
A 42-year-old male was admitted after being run over by a car while lying on the road. The patient’s initial hemodynamic parameters were stable (blood pressure: 120/80 mmHg; heart rate: 75 beats per min; temperature: 36.1°C; saturation: 98% on room air) with a Glasgow Coma Scale of 6 under the influence of alcohol intake. The patient had a liver cirrhosis (Child–Pugh class A) background with alcohol dependence and panic disorder. A scalp avulsion of 20 cm with exposure of a compressed skull fracture and multiple avulsions of the right anterior chest wall was noted in the primary survey. Abdominal tenderness was uncheckable. Computed tomography (CT) scans showed isolated AHC (Fig. 1) and a minor laceration in the right middle lobe of the lung. The injury severity score was 22.
Axial (A) and sagittal (B) views of the initial abdominal computed tomographic scans show isolated acute hemorrhagic cholecystitis with a dilatated extrahepatic common bile duct and cholelithiasis. Active extravasation of the contrast blush (arrowheads) into the lumen of the distended gallbladder is noted on the portal delayed phase. The liver parenchyma presents cirrhosis-like heterogeneities.
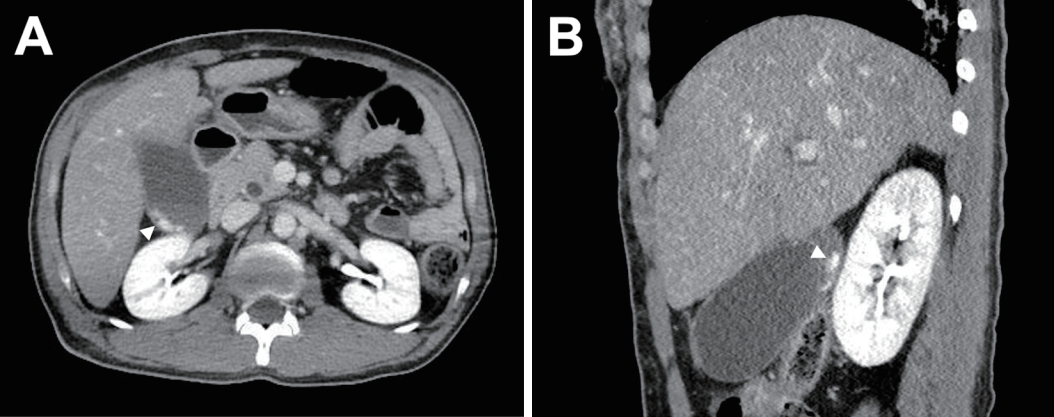
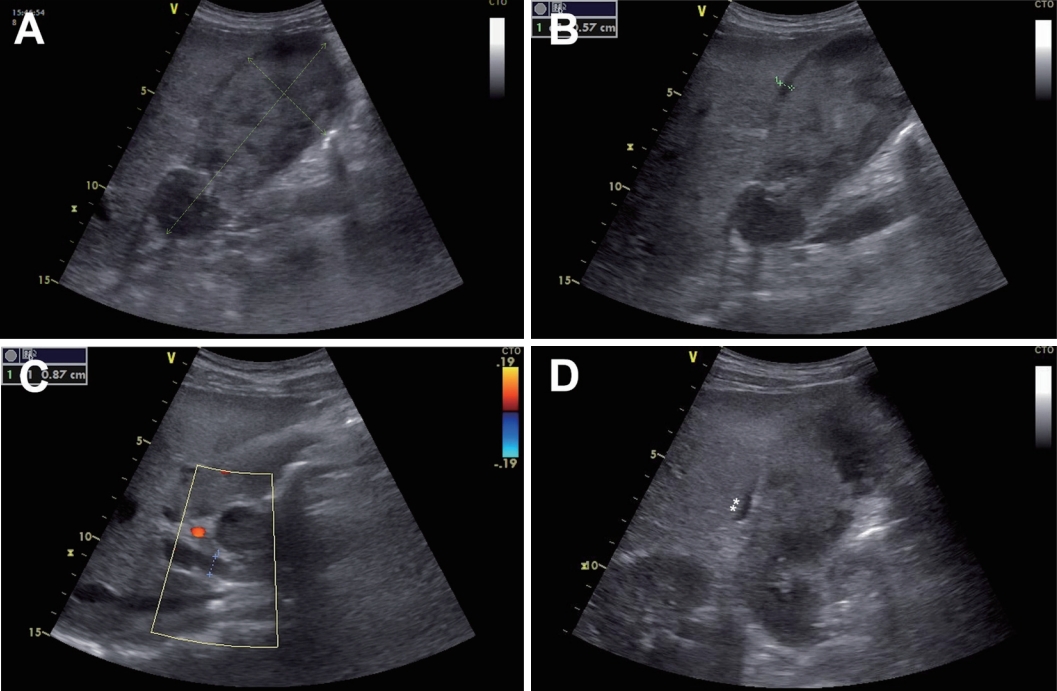
The patient became conscious the following day and complained of abdominal pain in the right upper quadrant and positive Murphy’s sign. The patient remained hemodynamically stable, but blood tests deteriorated (Table 1). Point-of-care ultrasound (POCUS) obtained with a Vivid S5 ultrasound (General Electric Healthcare, Chicago, IL, USA) revealed aggravated AHC (Fig. 2). Emergency laparoscopic cholecystectomy was performed based on the patient’s stable presentation (Figs. 3 and 4). The laparoscopy showed neither peritoneal fluid collection nor pericholecystic inflammation; thus, the dissection of the Calot’s triangle was uneventful. The patient made a complete recovery after the surgery, and the final pathologic diagnosis was transmural hemorrhagic infarction with chronic cholecystitis.
The findings of the point-of-care ultrasound. A notably large (118×73×50 mm) gallbladder with hyperechoic hematomas was visualized within the entire lumen (A). The content is nonshadowing and presents as clumps of echoes due to clot accumulations. The wall is 57-mm thick with edema (B). The dilatated proximal common bile duct of 87 mm (C) and a focal area of pericholecystic fluid (asterisks) is also noted (D).

Intraoperative photographs. The cirrhotic liver parenchyma and the grossly distended and tense gallbladder containing multifocal contusions without a perforation (A) were encountered along with a falciform ligament contusion (B).
Discussion
The rarity of the GB injuries from trauma is due to its anatomical location, embedded in the fossa on the liver surface and protected by the ribcage. The patient in the current study had a unique combination of multiple risk factors for traumatic AHC. Severe GB distension, which is caudally exceeding the roof (ribcage), can provide a reason for compression force to breach the protective anatomy. Alcoholism predisposes GB distension by increasing the tone of the sphincter of Oddi and raising the biliary tract pressure [1]. One report has proposed that the cirrhotic liver may exacerbate shear forces in the GB fossa by providing a stiff underlay [2]. Moreover, the GB polyp and the dilatated common bile duct may give clues to this patient’s long history of extrahepatic cholestasis before the accident.
Close follow-up physical examinations and serial imaging are essential to tailor further AHC management after trauma, and a delay may cause a loss of opportunity for timely and quality treatment. The CT is the most complete test for evaluating cholecystitis [3]. However, POCUS is also recommended because it can be frequently performed without the pressure of contrast injection, cost, or time consumption in patients with critical illnesses.
This case demonstrates that laparoscopic cholecystectomy is feasible in treating traumatic AHC with liver cirrhosis in a stable hemodynamic state. The definitive treatment for traumatic AHC is a cholecystectomy while a percutaneous cholecystostomy can be performed in patients with significant comorbidities [4]. However, cholecystostomy is not recommended because the hematomas mixed with bile create semisolid lumps that are hardly drained through a pigtail catheter of a small caliber. Recent studies reported that the cholecystectomy in patients with cirrhosis is feasible with low mortality and morbidity, especially in Child’s class A [5]. The cholecystostomy in patients with cirrhosis who have ascites showed a 14% risk of adverse events; thus, it is contraindicated [5].
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.