Introduction
Traumatic right-sided diaphragmatic hernia is a rare condition, with challenging diagnosis in some cases. Traditionally, diaphragmatic hernia is treated via direct repair using thoracotomy or laparotomy [1]. Recently, the development of minimally invasive surgery has led to the introduction of thoracoscopic or laparoscopic repair for diaphragmatic injury. Herein, we report a case of right-sided diaphragmatic injury that was successfully repaired via video-assisted thoracoscopic surgery (VATS).
Case presentation
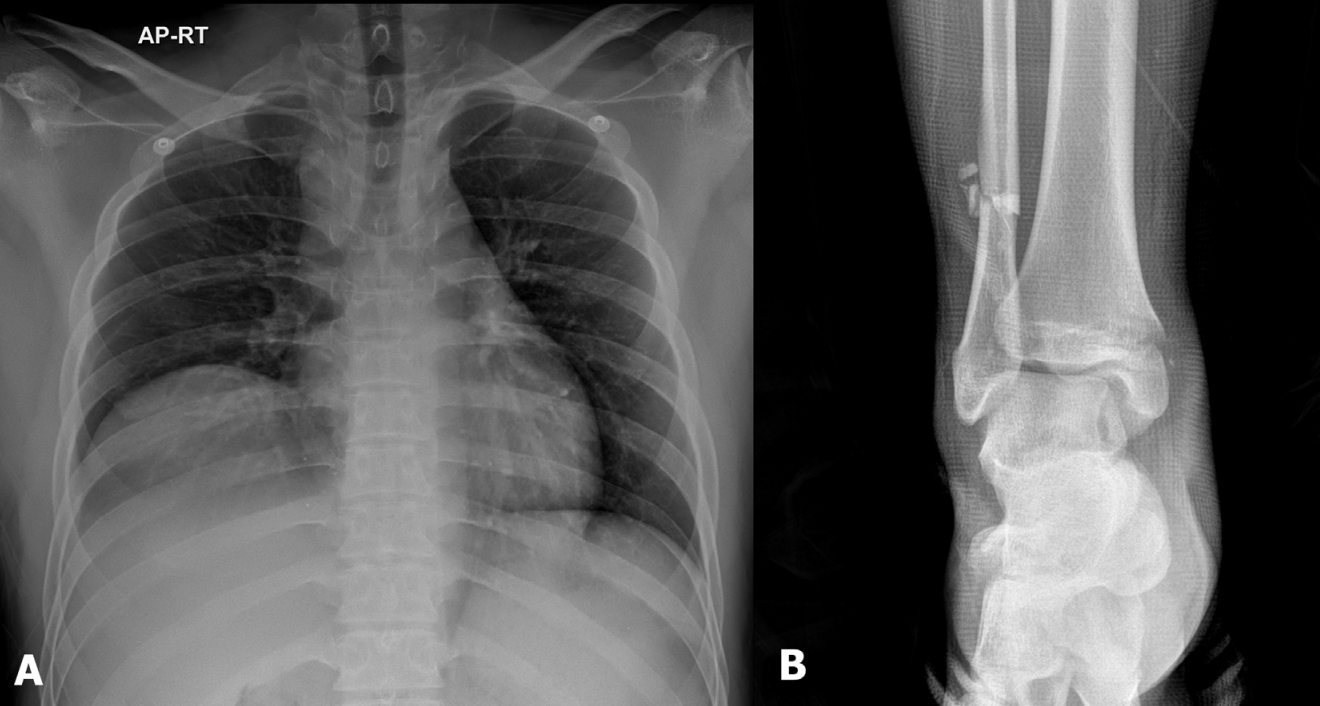
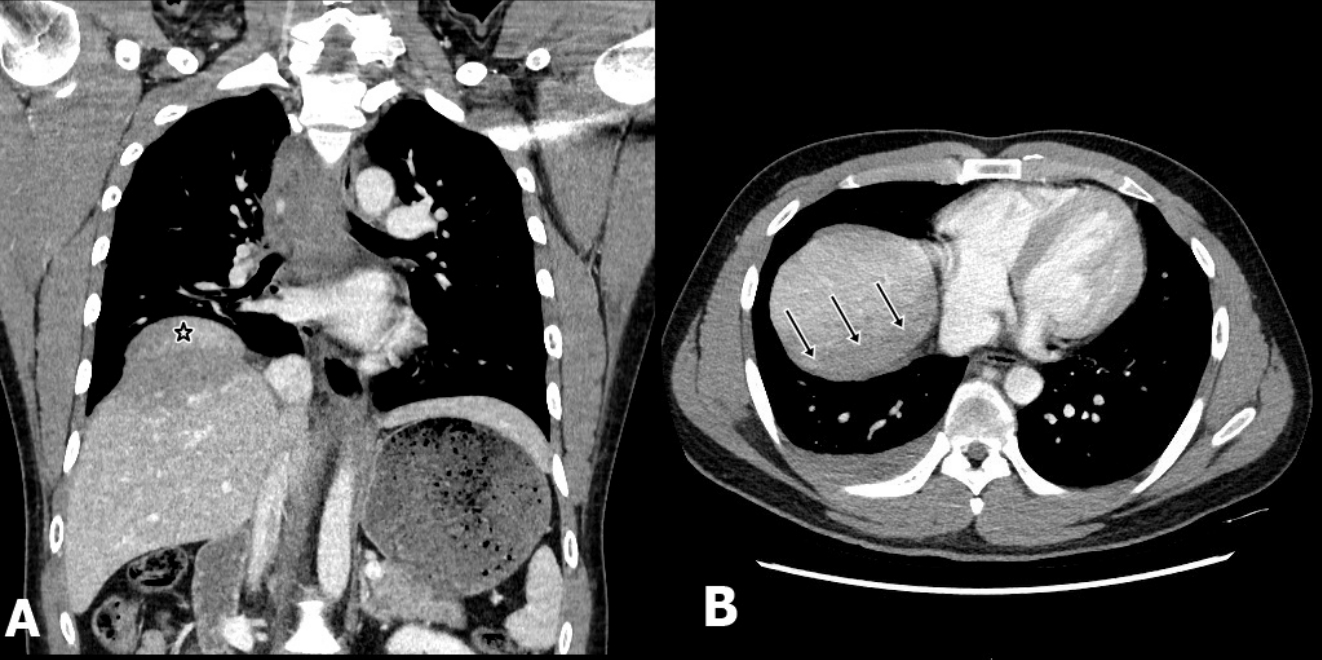
A 23-year-old man visited the trauma center after being involved in a traffic accident with complaints of chest pain and right ankle pain. His initial vital signs were stable, with no abnormal laboratory findings except for elevated levels of liver enzymes. Radiologic examination revealed minimal hemothorax and right hemidiaphragm elevation as well as bimalleolar fracture in the right ankle (Fig. 1). The presence of hump and band signs led to the suspicion of right-sided diaphragmatic injury (Fig. 2). Owing to this suspicion and because we wanted to perform a planned operation, such as VATS, the patient was admitted to the general ward for observation. The next day, he developed dyspnea, and liver enzyme levels were further elevated. Therefore, we decided to immediately perform VATS (Video 1). We observed bloody effusion (300 ml) and right-sided anterior diaphragmatic rupture (10-cm in length) along with superficial laceration on the exposed liver portion. Bleeding within the liver was controlled via electrocautery and use of hemostatic materials. The ruptured diaphragm was successfully repaired via VATS, and the patient was discharged on postoperative day 12 without any complications.
Operative Technique
Operation was performed under general anesthesia, and a double-lumen endotracheal tube was inserted. The patient was placed in the left lateral decubitus position, and a 5-mm, 30° videoscope was inserted via a 5-mm thoracoport. Initially, two additional ports were inserted (Fig. 3). After identifying the liver and diaphragm injuries, an additional port was inserted to retract the liver. Bleeding within the liver was controlled and then the diaphragm was repaired using interrupted horizontal mattress pledgeted nonabsorbable polypropylene sutures. We used pledgeted (polytetrafluoroethylene) sutures to prevent possible tissue tearing or damage.
Discussion
Blunt traumatic diaphragmatic injury (TDI) involves the left diaphragm (56%-86%) in the majority of cases and the right diaphragm only rarely [1]. Blunt TDI generally occurs during high-energy impact trauma; therefore, TDI diagnosis may be missed because of other severe injuries accompanying the TDI in patients with blunt trauma. However, multidetector computed tomography (MDCT) has a diagnostic accuracy of 95%, particularly when there is accompanying herniation [1]. There are several MDCT findings, such as collar sign, hump sign, band sign, and dependent viscera sign, indicative of TDI [2].
In general, laparotomy is advantageous in blunt TDI because associated abdominal injury can be verified, and reduction of herniated organs is easy with laparotomy. However, in cases of right-sided TDI, the liver is more likely to be injured, and adhesions may form between the margins of the ruptured diaphragm and the liver. The repair of right-sided injury is technically difficult via laparotomy, which requires mobilization of the friable liver. Therefore, open thoracotomy is considered a convenient approach for repair if there is no associated bowel injury [3]. In addition, a minimally invasive technique, such as VATS, could be more advantageous for the treatment of right-sided TDI.