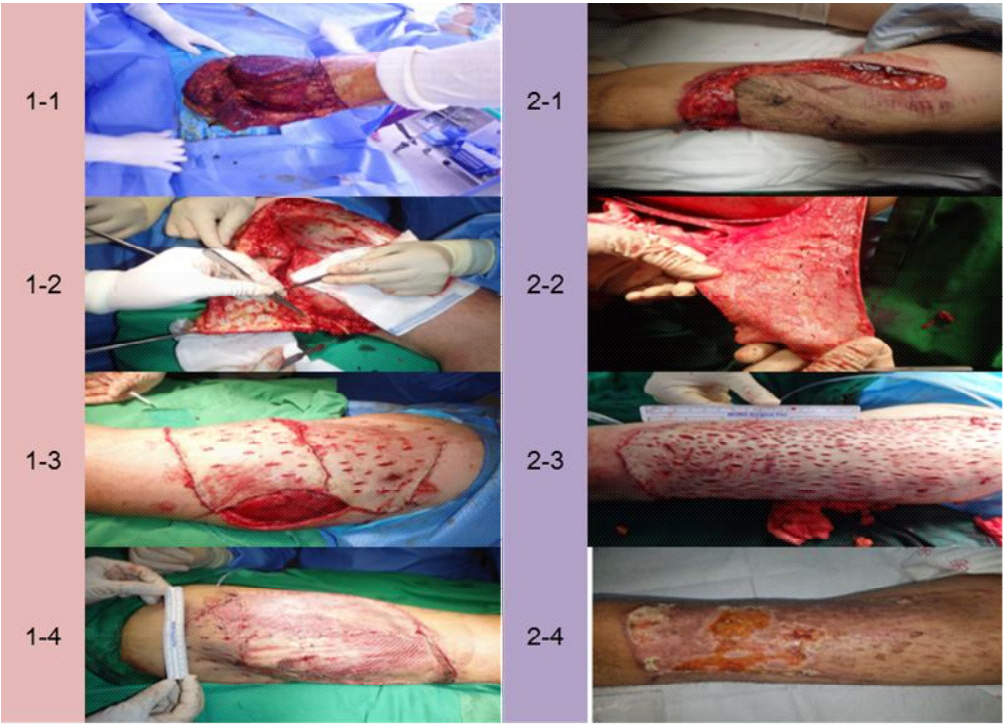
CASE I
A 34-year-old male struck by a steel ball was transferred to our trauma center. He suffered from a right ulnar fracture and a right femoral degloving injury sized approximately 20 × 30 cm, with a contaminated wound (Fig. 1-1.). After adequate debridement and irrigation, defatting with scalpels and the VERSAJET system (Smith and Nehew) was performed, followed by multiple small incisions for drainage of full-thickness skin graft to cover the denuded area (Fig. 1-2.). Negative-pressure wound therapy as applied after covering with Bactigras (Smith and Nehew). After 3 days, large necrotic areas were observed (Fig. 1-3.). At postoperative day 9, debridement and STSG were performed. At the 20-days follow-up postoperatively, the appearance had reduced to an acceptable level (Fig. 1-4).
CASE II
A 40-year-old male presented with multiple trauma including degloving injury with a contaminated wound on his left thigh (approximately 25 × 20 cm) (Fig. 2-1.) caused by a motorbike accident. His sartorius and rectus femoris were partially ruptured. Radical debridement and defatting were performed using scalpels and the VERSAJET system (Fig. 2-2.). To drain and prevent inordinate tension pressure of the covered skin graft, multiple incisions were made (Fig. 2-3.). In a similar previous case, Bactigras was used and NPWT was applied above the resurfaced skin graft. Upon hospitalization, debridement was performed in a ward owing to the detection of partial small necrotic lesions without infection. However, no further skin grafting was required for treatment.
DISCUSSION
Degloving injuries are caused because of entrapment between a moving object and a fixed surface, which separates the skin and subcutaneous tissue from the muscle and fascia [1]. The concept of resurfacing the denuded bed of such degloving lesions using a skin graft obtained from an avulsed flap is widely accepted [2]. However, it is difficult to treat an injury when deciding the surgical approach. Resurfacing and grafting of the avulsed flap is faster and more intuitive; however, this surgery often results in total or partial loss of the avulsed flap graft. Managing degloving injury of the lower extremities with immediate full-thickness skin grafting after radial debridement, defatting, and making multiple small incisions is feasible [3]. Both our cases were classified as non-circumferential degloving injury according to the classification by Arnez et al. [4]. Our first case required a secondary skin graft. However, in the second case, the affected site was treated without additional skin grafting. The reported cases are unique in that more multiple small incisions were considered to drain seroma or hematoma from the recipient bed.