|
 |
- Search
| Trauma Image and Procedure > Volume 7(1); 2022 > Article |
|
Abstract
Midline catheters (MCs), which are placed into the main veins of the upper arm, are a middle-ground option between peripheral venous catheters (PVCs) and central venous catheters (CVCs). New-generation MCs can be easily inserted at the bedside by a single operator and can be used until 29 days. Therefore, for a certain group of patients, new-generation MCs can potentially resolve the problems associated with CVCs and the need for recurrent PVC insertion. Therefore, this study aimed to present how to insert new-generation MCs.
Peripheral venous catheters (PVCs) are the most commonly used intravenous (IV) access to manage most patients, because they are simple to insert and have a minimal risk of problems [1]. However, for patients requiring long-term IV therapy, recurrent PVC insertions might be required to complete the course of treatment [2]. As a result, these patients frequently have central venous catheters (CVCs) placed; however, CVCs cause central-line-associated bloodstream infections [3] and increased risk of deep vein thrombosis [4].
Midline catheters (MCs), which are placed into the main veins of the upper arm, are middle-ground options between PVCs and CVCs. By definition, the MC tip should be situated distal to the shoulder, at or just below the axillary level. MCs cannot result in central-line-associated bloodstream infection since they are not CVCs [5]. Several studies reported that the prevalence of catheter-related bloodstream infections with MCs ranges from 0% to 0.9% (6). New-generation MCs, the all-in-one device with the modified Seldinger technique, have the needle, wire, and introducer in a combined unit for ease and speed in access. New-generation MCs are made of flexible polyurethane and are up to 80% softer inside the body to lessen harm to the vascular wall. Moreover, they can be used for up to 29 days, which has a longer duration than traditional PVCs. Therefore, for a certain group of patients, MCs can potentially resolve problems associated with CVCs and recurrent PVC insertion.
To find the best vein to cannulate in terms of the position, diameter, and depth, the patient’s forearm is supinated and evaluated with ultrasound (Fig. 3). Only >3-mm-diameter veins are considered. Veins above the elbow are more preferred over those in the upper mid-arm (cephalic, basilic, or brachial veins). Above the elbow, very near the axilla, the tourniquet is applied.
Antiseptic swabs with chlorhexidine, containing alcohol, are used to clean the puncture site. After removing the needle cover of the MCs, the needle is inserted into the vein using ultrasound. At this time, the blood should be checked through the catheter.
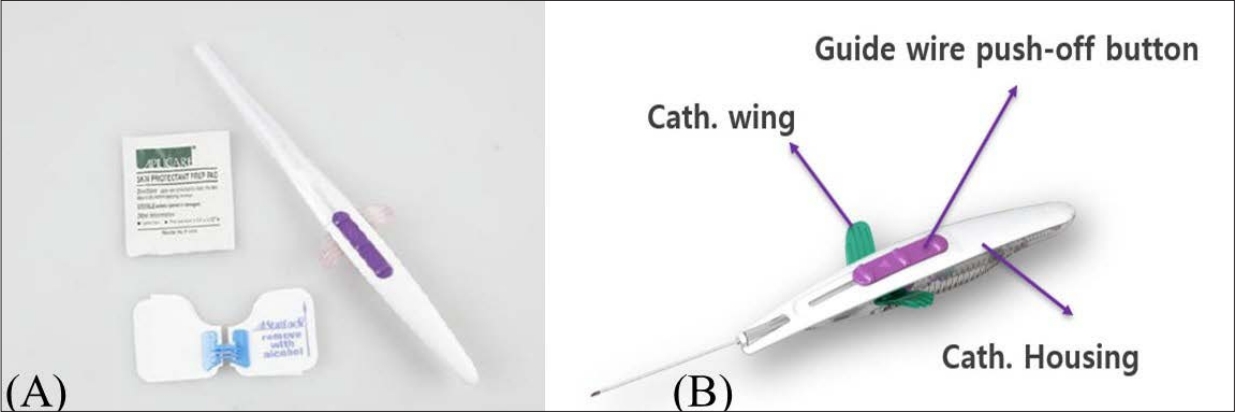
When blood reflux is confirmed in the catheter, the guidewire push-off (purple button) is pushed forward. When the guidewire is fully inserted, blood circulation decreases or stops. If the guidewire is not fully inserted, the catheter wing will not advance.
Holding a grip in place, the catheter is pushed into the vein using the catheter wing. The housing should always be held in a fixed position when advancing the catheter wing. Otherwise, the catheter will not be able to enter the vein, which may delay the procedure.
Hold the catheter handle securely in place and pull back to safely remove the housing and passive needle. By elevating the catheter wing while securing its end, the catheter wing can be removed. Immediately after removing the catheter wing, the extension set should be connected to the catheter hub and performed flushing.
According to each hospital’s guidelines, the catheter insertion site should be dressed. If you are using a PowerGlide Pro™ Midline Catheter, using a StatLock® device retainer is recommended (Bard Acess System Inc., Salt Lake City, UT, USA) (Fig. 4).
New-generation MCs can potentially resolve the problems associated with both repetitive catheter insertions and resource demands posed by PVCs and CVCs, respectively.
Moreover, the new-generation MC is an all-in-one type of device that can be easily inserted through ultrasound. It can be implanted without ultrasound if the blood vessel is properly palpable.
Supplementary material
Supplementary data including one video can be found with this article online at www.traumaimpro.org.
Fig. 1.
Midline catheter (MC) preparation: gloves, a dressing vein using ultrasound. At this time, the blood should be kit and a MC kit.
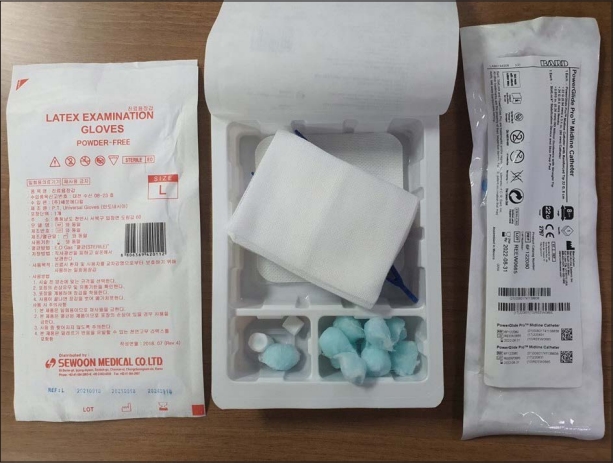
Fig. 2.
(A) The PowerGlide ProTM Midline Catheter kit consists of PowerGlide ProTM Midline Catheter, StatLock® IV ultra stabilization device, and a skin preparation pad. (B) PowerGlide ProTM Midline Catheter body consists of the needle, a catheter housing, a catheter wing, and a guidewire push-off button.
REFERENCES
1. Rickard CM, Webster J, Wallis MC, Marsh N, McGrail MR, French V, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-74.


2. Adams DZ, Little A, Vinsant C, Khandelwal S. The midline catheter: a clinical review. J Emerg Med. 2016;51:252-8.


3. Dawson RL. Midline catheters: an essential tool in CLABSI reduction. infection control today; Available:https://www.infectioncontroltoday.com/clabsi/midline-catheters-essential-toolclabsi-reduction [Accessed 24 Jun 2018].
4. Chopra V, Anand S, Hickner A, Buist M, Rogers MA, Saint S, et al. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta-analysis. Lancet. 2013;382(9889):311-25.


- TOOLS