Bedside peripherally inserted central catheter placement: focus on the procedure
Article information
Abstract
A peripherally inserted central catheter (PICC) provides long-term central venous access through a peripheral vein in an upper extremity. A trained physician should insert a PICC, but any trained medical professional, such as a specially trained nurse, can perform an insertion. Appropriate PICC placement reduces complications, such as malposition and malfunction of the catheter, venous thrombosis, and infections, and overall catheter performance is better. Complications depend mainly on the adequacy of venous puncture or the positioning of the catheter tip. Better PICC performance depends on learning accurate techniques for insertion. Here, the overall procedure for bedside ultrasonography-guided PICC placement, including patient positioning, catheter preparation, venous assessment and measurement, overall technique, and catheter tip positioning, is described.
Introduction
Given a high incidence of adverse events in critically ill patients during intra-hospital transport, acceptable outcomes for bedside placement of a peripherally inserted central catheter (PICC) in the intensive care unit have been in the spotlight since 2000 [1]. Compared with other central vascular access devices, such as conventional central venous catheters, PICCs usually carry a low risk of pneumothorax, local hematoma, and catheter-related bloodstream infections [2]. However, improperly inserted PICCs can result in complications, such as malposition, migration, occlusion, infection, and venous thrombosis, which can be lethal in critically ill patients [2]. An accurate technical procedure for PICC placement can improve overall catheter performance. Here, a precise procedure for bedside ultrasonography-guided PICC placement, including patient positioning, venous assessment and measurement, preparation of the vascular device, overall technique, and positioning of the catheter tip, is described.
Methods
Patient positioning and preparation
The patient is positioned supine, with arms abducted >90°, head turned toward the ipsilateral arm, and chin tucked (Fig. 1). The head and neck should be immobilized, if the patient has any known or suspected abnormality of the cervical spine. The ultrasound machine is placed on the opposite side of the arm where the PICC is inserted. A tourniquet is prepared around the upper arm close to the axilla. For skin preparation, chlorhexidine–alcohol is applied to about 60% of the upper arm’s circumference from axilla to elbow.
Venous assessment and measurement
The basilic vein is assessed by ultrasonography using a 12 MHz linear array probe to locate an optimal puncture site in the mid-upper arm area (“green zone”), 7-14 cm proximal to the medial epicondyle [3]. When the basilic vein is unavailable, the brachial or cephalic vein can be used. However, a puncture on the brachial vein should be avoided whenever possible, as it runs along the brachial artery.
The transverse diameter of the relevant vein at the insertion point is measured under ultrasound guidance (Fig. 2). Based on the rule that the three-dimensional percentage of area for a catheter is under 45%, veins with a diameter of 3 mm or more are considered suitable for 5 Fr double-lumen catheters, and veins of 3.5 mm or more for 6 Fr double-lumen catheters [4]. The catheter length for optimal positioning is determined by adding the distances from the puncture site to the lower border of the mid-clavicle, from the mid-clavicle to the sternoclavicular junction, and from the sternoclavicular junction to the third intercostal space in the right parasternal border (Fig. 3). Similar measurements are made in the case of left-side insertion (Fig. 4).

(A) Color doppler ultrasonography shows the distinct flows of the basilic vein (BV), brachial artery (BrA), and brachial vein (BrV). (B) The transverse diameter of the basilic vein is measured at 3.5 mm by ultrasonography. (C) Skin markings for the basilic vein (BA.v.), brachial artery (Br.a.), and brachial vein (Br.v.) are shown on the right upper arm.

Measuring for optimal catheter positioning (right arm). (A) Surface anatomy is marked on the right upper arm and upper chest. (B) The distances from the puncture site in the right upper arm to under the right mid-clavicle, (C) from the midclavicle to the right sternoclavicular junction, and (D) from the sternoclavicular junction to the third intercostal space at the right parasternal border are measured.
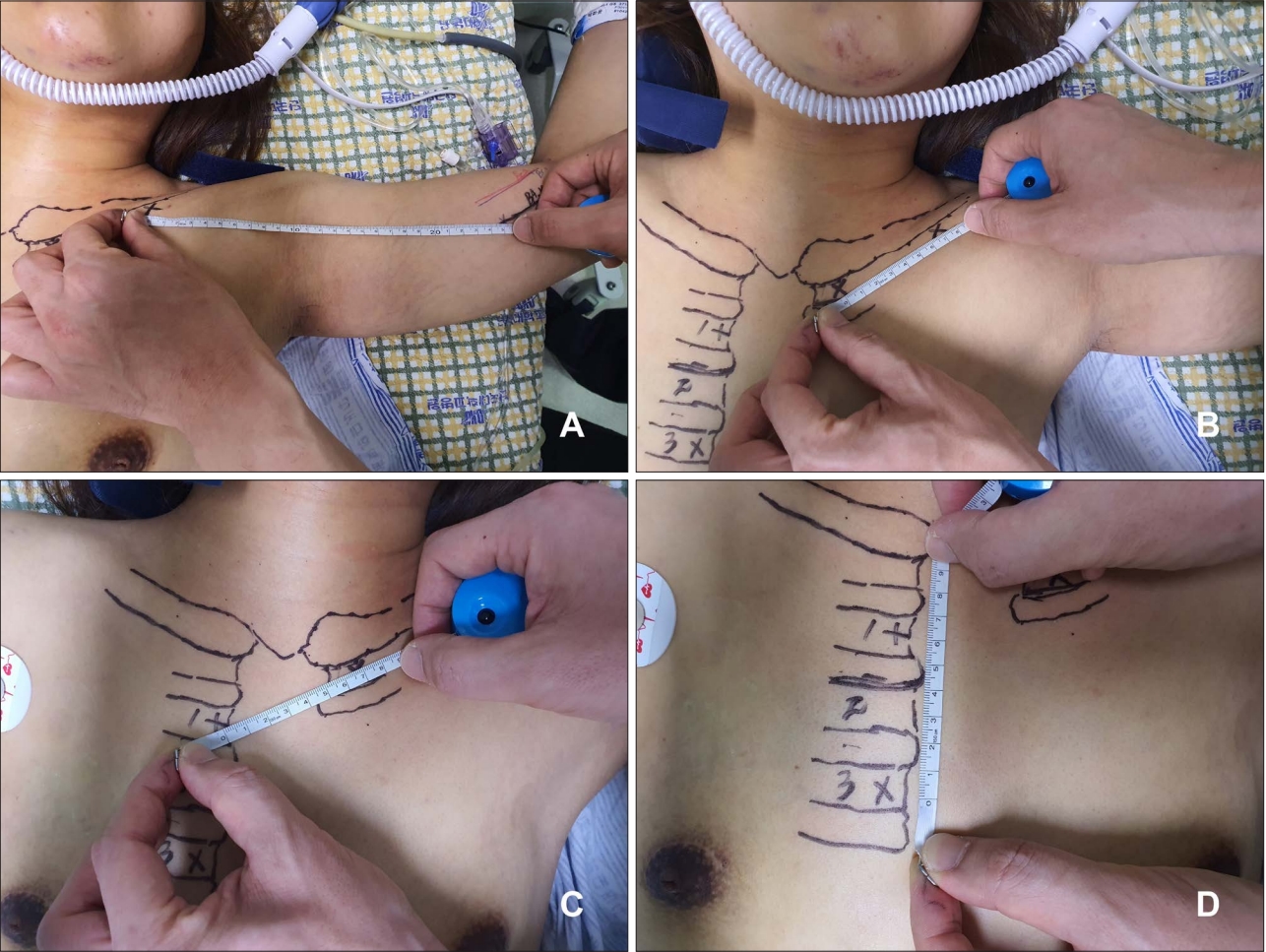
Measuring for optimal catheter positioning (left arm). (A) The distances from the puncture site in the left upper arm to the point under the left mid-clavicle, (B) from the mid-clavicle to the left sternoclavicular junction, (C) from the sternoclavicular junction to the first intercostal space at the right parasternal border, and (D) from the first intercostal space to the third intercostal space are measured.
Preparation of the PICC
The over-the-wire technique is used for a 5 Fr double-lumen Kimal PICC (Kimal PLC, Uxbridge, UK). Video 1 shows the preparation of the catheter before the insertion procedure. The catheter is cut to the measured length after both lumens have been flushed with saline.
Procedure
The operator wears a surgical gown and gloves, and surgical drapes are laid over the patient to achieve maximal barrier precautions. The ultrasound probe and cable are covered with a sterile sleeve-like drape. The tourniquet around the upper arm is tightened. Video 2 shows the next steps in the procedure:
1. The basilic vein puncture is performed using a 21-gauge micropuncture needle (7 cm in length) under ultrasound guidance.
2. A 0.018-inch guidewire (50 cm in length) is introduced into the vein through the needle.
3. The location of the guidewire in the vein is confirmed by ultrasonography, and the tourniquet is released.
4. The needle is then withdrawn, and 2% lidocaine is injected into the skin around the puncture point.
5. An incision to accommodate the sheath microintroducer is made at the puncture point using a scalpel.
6. With its inner dilator, the short peel-away sheath microintroducer is advanced along the guidewire into the vein, with the wire and dilator removed.
7. The 5 Fr catheter (55 cm in original length) is introduced into the vein through the sheath. If the patient’s head cannot be turned ipsilaterally, the catheter can be advanced further while pressure is applied by the operator’s left hand near the confluence of the ipsilateral internal jugular vein (IJV) and the subclavian vein.
8. The sheath is peeled away and removed after absence of the catheter in the ipsilateral IJV is confirmed by ultrasonography. If the catheter is in the IJV, it is pulled back and advanced again.
9. Of two lumens, blood reflux through the red lumen in which the stylet (80 cm in length) is not mounted is checked using a syringe at first. The lumen is then flushed with saline.
10. After the three-way connector holding the stylet in the blue lumen has been removed, blood reflux is again checked, and the lumen is flushed.
11. Both lumens are locked with the disinfection caps.
12. The hub of the PICC is secured using a sutureless stabilization device (in this case, a StatLock® PICC Plus: Bard Venetec International, San Diego, CA, USA). A transparent gel pad integrating chlorhexidine gluconate is used as a dressing.
Positioning of the catheter tip
Post-procedural chest radiography must verify that the catheter tip is correctly positioned. Although no consensus has been reached about the correct position for the tip of a PICC, US Food and Drug Administration guidelines [5] suggest the inferior third of the superior vena cava, and European guidelines [2] recommend the right atrium.
Malfunctions of the central catheter can be minimized by locating the catheter tip as close to the cavoatrial junction as possible or slightly inside the right atrium [6]. Compared with using the carina as a landmark, cardiac silhouettes are considered unreliable for positioning [7]. Hence, a catheter tip located from the tracheal carina to 5 cm below the carina is regarded as an acceptable position on anteroposterior radiography images (Fig. 5A and B) [8,9]. Malposition of the PICC can appear in several notable places or forms, such in the ipsilateral or contralateral IJV, or with catheter kinking (Fig. 5C–F).

A peripherally inserted central catheter (PICC) is positioned on anteroposterior chest radiography. (A) The optimal position for the catheter tip is considered in the region from the tracheal carina to 5 cm below the carina. SVC, superior vena cava; CAJ, cavoatrial junction. (B) Optimal positioning of a catheter tip in the cavoatrial junction. The PICC is considered malpositioned if the tip (white arrow) is positioned (C) in the ipsilateral internal jugular vein (IJV), (D) coiled in the upper superior vena cava, or (E) positioned in the contralateral IJV, or (F) if the catheter shaft (white arrow) is tortile in the ipsilateral axillary vein and the tip (black arrow) is positioned in the ipsilateral subclavian vein.
Discussion
For patients who require long-term vascular access, bedside PICC placement can be an excellent option with a high success rate [1]. Undesirable positioning of a PICC can be associated with complications such as arrhythmias, thrombosis, phlebitis, and cardiac tamponade [9–11]. Currently, various techniques for optimal positioning of a PICC have been published, including fluoroscopy-guided, magnetic tracking, electrocardiogram-based, and blind [1,12]. Although fluoroscopy-guided insertion is considered the gold standard, the blind technique with no guidance is the most popular in the intensive care unit because it can be used at the bedside with no special technology. If implemented according to the guidelines and principles for correct positioning of a catheter tip, bedside ultrasonography-guided PICC placement is a safe technique that can be used with minimal complications in the intensive care unit.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Supplementary material
Supplementary data including one video can be found with this article online at www.traumaimpro.org.
Video 1.
A video recording shows preparation of the peripherally inserted central catheter kit.
Video 2.
A video recording shows the general procedure for placing a peripherally inserted central catheter.
